ARE YOU UNDER VALUING YOUR CLIENT’S CASE? This is the first article in a series that I will be bringing to you over the next 8 months. In this first article I hope to shed light on a simple misconception of whiplash and help you determine if your client or claimant has 5-8% impairment or 25-28% impairment. (1) The latter will allow for increased settlement demands and should improve settlement offers. It also will help you weed out those few that are trying to “pull one over” on the system, which cost all of us in the end, as the testing cannot be faked.
This is the first article in a series that I will be bringing to you over the next 8 months. In this first article I hope to shed light on a simple misconception of whiplash and help you determine if your client or claimant has 5-8% impairment or 25-28% impairment. (1) The latter will allow for increased settlement demands and should improve settlement offers. It also will help you weed out those few that are trying to “pull one over” on the system, which cost all of us in the end, as the testing cannot be faked.
The Stigma
Whiplash is an outdated term, but we all are familiar with it. Most often the whiplash injury is thought of as a rear end impact flexion/extension injury. This term is dated and we should avoid using it outside of a laymen conversion. Cervical strain injuries after a MVC should be referred to as a cervical acceleration/deceleration (CAD) injury. This eliminates the single motion of injury and is more accurate for frontal impact, side impact, or rear end collisions. (2)
Many people who have never experienced a CAD injury personally or had a close family member experience it, talk about this type of injury with a wink and a smile, right? Let’s look at why. The patient sits in front of his or her physician 12 months after the motor vehicle crash (MVC) and tells them how much they hurt, with complaints of neck pain, headaches, mid-back pain, and even dizziness. Yet in the physical exam the neck range of motion is normal or near normal and they look good. Many of them are working, but claim the pain is worse with activity and some even expect us to believe it hurts while sitting still or driving, despite their normal MRI and plain film x-ray findings. In the past, this type of patient would be looked upon as a malinger or a magnifier, embellishing the symptoms trying to make a quick “payday or win the lottery”.
Which is it? Cervical strain or AOMSI
Patients do have neck strain CAD injuries causing pain or soreness, but these often recover in 2-12 weeks. (3) This cervical strain injury would receive a whole person impairment of 0-5% (1) and is the classification that I see both insurance adjustors and some of my patients’ attorneys place all CAD injuries. There is however, the patients that have more than mild strains to the muscles. This patient is that confusing case that just will not get better, whose MRI is normal or the MRI reveals a degenerative disc (watch for the disc dilemma in a future issue), or normal CT scans, as well as normal radiographs. It is important to remember that most radiologist read plain film radiographs for pathology and not mechanical faults like AOMSI. Do not believe me? Call the radiologist listed at the bottom of your next normal cervical x-ray report and ask them to explain first, AOMSI to you and second, when is the last time they measured a film using the criteria explained in the Guides to the Evaluation of Permanent Impairment, 5th edition.
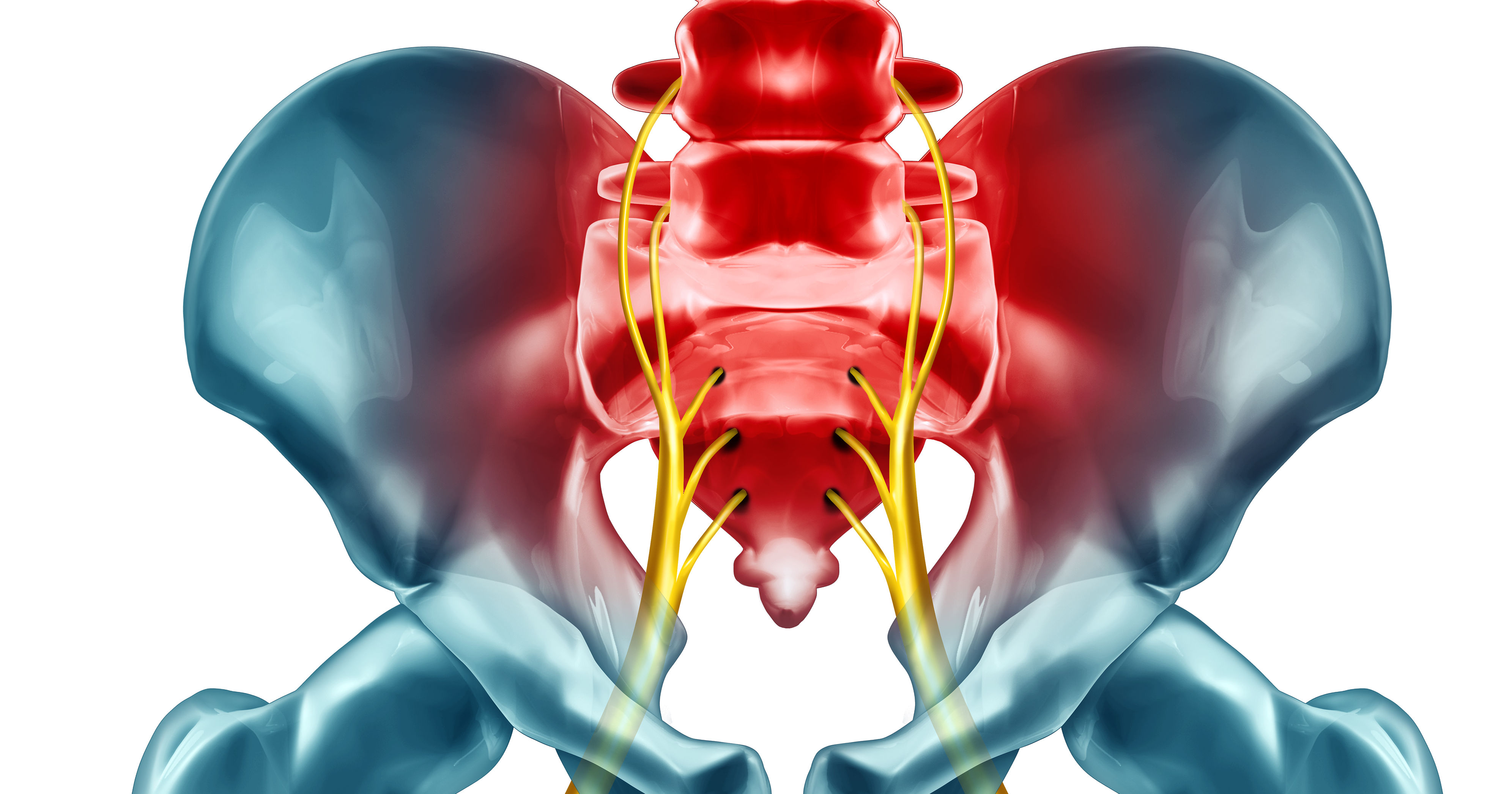
Alteration of Motion Segment Integrity (AOMSI)
In my experience this term is often one that many attorneys and doctors have never heard of or do not completely understand. AOMSI is the alteration of motion segment integrity, meaning an increased translation (hypermobility) or angular motion, or decreased motion as in a spinal fusion. (1) AOMSI is determined by computerized line drawings on cervical stress films, more specifically flexion and extension views, as you would see in the medical records. The design of the test is to stress the injured structures that support the spine and as a result this test often causes a reproduction of the client/claimant’s complaints. There is a second way to determine this injury known as digital motion radiographs (DMX), which is video fluoroscopy of the spine. While this test looks great, because you see full motion of the spine, the radiologist will read this study at the end points of range of motion as a still shot; the same method of analysis as in plain film measurements as described in the Guides to the Evaluation of Permanent Impairment, 5th edition. I have found the advantage is that the person performing the DMX understands that the client/claimant has to move to fully to the end range of motion for accurate measurements and the studies are both analyzed and read for pathology by a radiologist who understands the findings of AOMSI. If radiographs are performed elsewhere, then there is a radiologist who reads for pathology, and then the films would have to be referred to a second radiologist for the proper analysis.
How many of your CAD injured client/claimant’s with pain longer than 3 months have stress films performed? Is the provider of this injured person looking for this injury? Does the radiologist know and perform the proper analysis to make the correct diagnosis?
Action steps
1. Ask questions to the client and to the provider. Ongoing pain longer than 8-12 weeks post MVC, in the absence of neurological compromise or fracture, stress radiographs or video fluoroscopy might provide your answer.
2. Seek out someone who understands the injury. If you are not sure if the provider “gets it” or the claimant is not being truthful, then request an independent chiropractic/medical examination. Just make sure the examiner understands these types of injuries. Although frustrating, I had to refer a patient last year to a surgeon out of state who understood this injury and performed the necessary stabilization surgery.
3. Findings of AOMSI need to be identified either as a probable pre-existing condition or a probable a new condition? Experienced clinicians will be able to advise you on this matter.
Evaluating AOMSI will help you separate those temporary CAD injuries from the permanent CAD injuries and determine the real value of your case.
References
Cocchiarell, L., Andersson, G. (2001). AMA Guides to the Evaluation of Permanent Impairment, 5th edition: The American Medical Association
Croft, A., Foreman, S. (2002) Whiplash Injuries: The cervical acceleration/deceleration syndrome: Lippincott Williams & Wilkins
Carroll, L., Holm, L., Hogg-Johnson S, et al. Course and prognostic factors for neck pain in whiplash-associated disorders (WAD): Results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and its Associated Disorders. Spine 2008;33(4 Suppl):S83-92.


Dr. Linton
At Linton Spine & Joint Chiropractic Center, we offer a broad range of treatment options and services to our Mt. Sterling patients. Dr. Linton will work with you to identify which treatments will be the most effective and fitting for your specific needs.